Updated June 2024Pain come and goes, and sometimes, it sticks around. Chronic pain can have a number of different causes and range from annoying to debilitating. Sometimes, after the original source of pain is resolved, the body can continue to feel discomfort due to nervous system's memory.
Often pain isn’t localized to just the original site of injury. If you hurt your knee, you may not be able to bend your leg, and when you have to pick stuff up from the floor, you use your back, which is stressful to your spinal muscles- now you have back pain as well as knee pain. This happens to animals too. As pets compensate for a painful body part, they may stress or even injure other areas- muscles and ligaments are especially susceptible to this type of strain. A single painful event which eventually heals can lead to chronic pain too, such as the case in urinary tract problems, torn ligaments, or even after surgical procedures. A multi-modal approach involves physical therapies, supplements, medication and adjusting your pet's environment. Remember that helping your pet manage aches and pains is a team approach starting with your pet, your vet, and you. No time to read this article? Look at this video for 5 tips you can do at home, courtesy of Dr Roark, vet and comedian. 
Read on!
1. Recognizing Pain Understanding your dog or cat: The Indoor Pet Initiative Be a Cat Champion: Cat Friendly Home 2. Comfort Management at home 3. Weight 4. Exercise 5. Supplements 6. Heat & Cold Therapy 7. Manual and Complementary Therapies: Laser, Acupuncture, Massage, PT and more. 8. Medication Help me medicate my cat! Tips for your veterinarian and you. |
1. Recognizing Pain
Pain is the main reason why we humans go see our doctors. That is not the case with our pets, because as their caretakers, we often fall short of recognizing the subtle signs of pain.
Pets are not furry humans and they express pain very differently than we do. Animals hide pain. It is a survival instinct that they retain from their wild ancestors. Humans have to learn to recognize pain in animals, especially when it develops over time as most animals will not cry, whine, or otherwise show you they are in chronic pain. A dog that no longer gets up when the doorbell rings , a cat pees outside the litter box, is quicker to bite or scratch, or no longer uses the scratching post or any change in your pet's regular behavior can indicate pain. Some studies suggest that more than half of cats older than 6 yrs of age have issues in one or more joints and even some dogs as young as one year of age show evidence of arthritis! A 2012 study found 90% of cats studied older than 12 years had evidence of arthritis on x-rays!
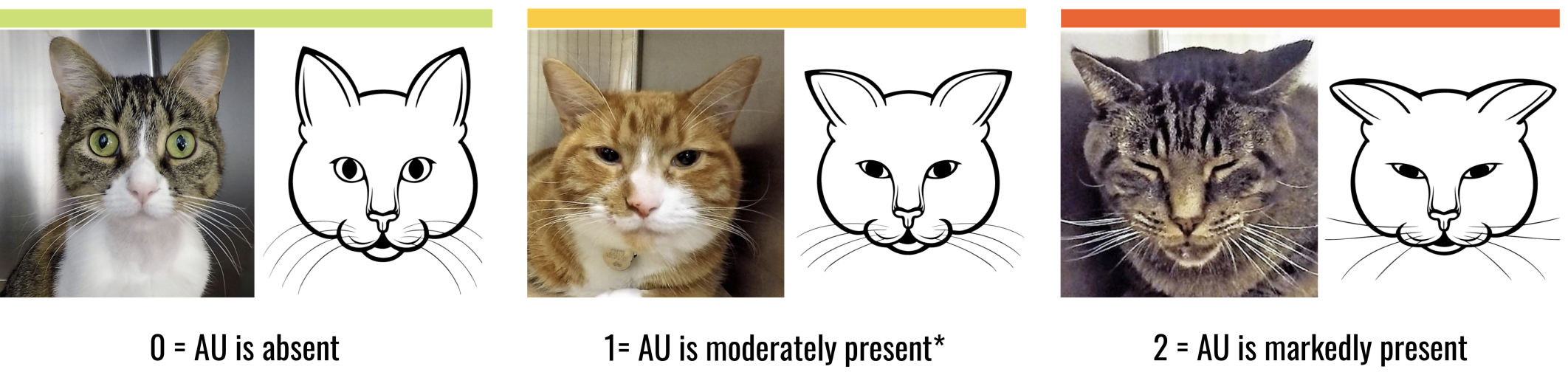
Click on the video and image to learn the signals your cat may be giving you:
Pain is the main reason why we humans go see our doctors. That is not the case with our pets, because as their caretakers, we often fall short of recognizing the subtle signs of pain.
Pets are not furry humans and they express pain very differently than we do. Animals hide pain. It is a survival instinct that they retain from their wild ancestors. Humans have to learn to recognize pain in animals, especially when it develops over time as most animals will not cry, whine, or otherwise show you they are in chronic pain. A dog that no longer gets up when the doorbell rings , a cat pees outside the litter box, is quicker to bite or scratch, or no longer uses the scratching post or any change in your pet's regular behavior can indicate pain. Some studies suggest that more than half of cats older than 6 yrs of age have issues in one or more joints and even some dogs as young as one year of age show evidence of arthritis! A 2012 study found 90% of cats studied older than 12 years had evidence of arthritis on x-rays!
Click on the video and image to learn the signals your cat may be giving you:

The International Veterinary Academy of Pain Management (IVAPM) has a checklist to help you assess pain in animals:
Click on the image for the link!!!
If you think your pet is in pain or you notice a behavior change, trust that instinct and explain to your vet why you think so, even if you can't pinpoint the exact problem. Don't forget that pets have their individual personalities that may make it more, or less, obvious when they are experiencing discomfort or pain. Trust your vet if he or she tells you that pain is present, even if you don't think you see it, you will recognize a difference once it is addressed.
To recognize what is abnormal in animals, consider what is normal. You might be surprised by how different every species experiences the same environment. Check out the Indoor Pet Initiative for some cool things that go on in your pet's brain and how you can help.
Most animals will show signs so subtle, their pain may go unrecognized for years and steps to lessen the pain or slow down the progression are delayed. Pain is its own medical condition, not just a symptom. It deserves its own time commitment. Relieving your pet’s pain is as crucial to address in the case of chronic injury as it is to an acute one. A urinary tract infection hurts. So does an ear infection, a herniated disc, or an ACL tear - those tend to be acute pain and veterinarians address this immediately at the time of diagnosis. Soreness and pain that accumulates as the body ages are harder to spot and often involve a much longer conversation with your vet. It is important to recognize the length of time you and your vet need to properly diagnose and create a plan for therapy. Also know that the plan will likely be adjusted depending on your pet’s response to therapy. The issue of your pet being in pain is not something you should tag on in the manner of "by the way can you check this while we are here for something else." If pain management isn't your vet's strong suit (we can't all be experts in everything) then ask him or her if there is anyone in or outside their practice they can refer you to for a consult. There are veterinary pain specialists who deal just in this very important issue.
Back to Table of Contents
2. Management at home
Arthritic pets have much more difficulty stabilizing themselves: hardwood/tile floors or deep cushioned beds, can be a challenge- like walking over a patch of ice or walking across a trampoline for us. Arthritic kitties have a much harder time getting to their safe zone on a perch, or navigating around a small litter box or one with higher edges to step over. The stress of not being able to use their body or their environment the way they see fit, can manifest as behavioral changes (and problems such as peeing outside the litterbox, overgrooming, or no longer allowing you to trim nails.)
A basic list to get your started- many of these tips are for both dogs and cats!
- Place area rugs or runners on non carpeted floors. (Use yoga mats for traction)
- Raise food and water bowls to your pet's shoulder height to decrease the stress on neck, front legs and spine. Area rugs or standing mats at the food/water bowl are helpful.
-Provide steps to the bed and steps into the car. (lots of tips on the internet!)
- Consider memory foam mattress pet beds: initially firm, it becomes softer as it adjusts to your pet's body heat. Help your pet out of its comfy bed onto stable ground if needed.
-Use a harness to help dogs up and down stairs or those that have a hard time getting around- these exist for both hind and front end support. I really like the Help’em Up Harness.
- Offer a heating or self heating pads for your kitty to lay on: make sure you purchase one made specifically for pets as the product needs to take on your pet's claws, fur, and increased chances of exposure to wet conditions. A small sheepskin rug are great non electrical options. IKEA has both real sheepskin and vegan/manmade alternative.
- Keep nails trimmed so they don't catch on carpeting/furniture which can yank on painful joints. Long nails can cause excessive strain on arthritic digits and cause your pet to have a harder time balancing. Trim hair between paw pads so the pads can grip flooring better. Consider using rubber nail covers to help with traction on slippery floors. Soft Paws and Paw Friction are popular options. Your groomer or vet may have suggestions. Pets with chronic pain may no longer allow you to trim their nails, so be suspicious if you start to get a growl or your pet struggles during previously uneventful nail trims.
- Get a large, uncovered litter box with a low step entrance, place a step to the litter box or cut an "entrance" so your cat doesn't have to jump over the side. I often recommend those under-the-bed plastic containers as they are low and wide/long so arthritic kitties have a much easier time turning around in them. Sometimes higher sides are needed as some kitties can't squat very well and pee over the edge...for those, get a high walled container and cut an entrance on one of the sides.
-Provide a litter box in areas where your cat doesn’t have to go up and down stairs.
Back to Table of Contents
3. Weight management and nutrition
A study showed that an obese person is 100% more likely to have chronic pain than a lean person. Overweight pets have a shorter span (average of two years less, according to a study on overweight Labradors). Quality of life is greatly affected by weight and many overweight pets are euthanized due to their inability to stand or walk comfortably, or because they are having accidents in the house as going outdoors or squatting becomes too painful, in spite of being otherwise relatively healthy. Being strict about caloric intake is one of the most important things you can do as a pet parent. Start before the pain shows up. If your pet becomes overweight, recognize the urgency in getting him or her back to a healthy weight. Every excess pound (or ounce in small animals) your pet carries exponentially increases pain. Proper nutrition is also of great importance: building blocks needed for maximizing healing and minimizing damage to our cells come from a proper diet. Diets may need to be customized to a animal's specific health needs. Food labels can be VERY confusing (see my blog!) Weight loss can be difficult for pets who have arthritis so medication, supplements and physical therapies have to come into play to manage pain.
A study showed that an obese person is 100% more likely to have chronic pain than a lean person. Overweight pets have a shorter span (average of two years less, according to a study on overweight Labradors). Quality of life is greatly affected by weight and many overweight pets are euthanized due to their inability to stand or walk comfortably, or because they are having accidents in the house as going outdoors or squatting becomes too painful, in spite of being otherwise relatively healthy. Being strict about caloric intake is one of the most important things you can do as a pet parent. Start before the pain shows up. If your pet becomes overweight, recognize the urgency in getting him or her back to a healthy weight. Every excess pound (or ounce in small animals) your pet carries exponentially increases pain. Proper nutrition is also of great importance: building blocks needed for maximizing healing and minimizing damage to our cells come from a proper diet. Diets may need to be customized to a animal's specific health needs. Food labels can be VERY confusing (see my blog!) Weight loss can be difficult for pets who have arthritis so medication, supplements and physical therapies have to come into play to manage pain.
4. Exercise
Proper exercise, such as a series of short walks or passive range of motion exercises while s/he is resting or as part of play is a very important part of musculoskeletal pain management. I see people dragging their old pets by their leash- would you drag your dear grandpa down the street if he couldn’t keep up with you? If you need to run errands, leave your old friend at home, then take a bit of down time for yourself and use your pet's exercise time to recharge your mind and get some fresh air (ok ,ok, check Facebook on your phone). Time your walks so your dog doesn't get tired before getting back home. Note the signs of your dog getting tired on a walk (increased up and down motion of the head, nails dragging more, stopping and laying down ). Know your pet’s limit and make sure get home before it is reached. Your cat's shaky legs while squatting in the litter box, or missing the litter box entirely can be signs of discomfort. Exercise relieves stiffness and increases/maintains mobility but make sure you provide it without causing pain or exhaustion.
Back to Table of Contents
Proper exercise, such as a series of short walks or passive range of motion exercises while s/he is resting or as part of play is a very important part of musculoskeletal pain management. I see people dragging their old pets by their leash- would you drag your dear grandpa down the street if he couldn’t keep up with you? If you need to run errands, leave your old friend at home, then take a bit of down time for yourself and use your pet's exercise time to recharge your mind and get some fresh air (ok ,ok, check Facebook on your phone). Time your walks so your dog doesn't get tired before getting back home. Note the signs of your dog getting tired on a walk (increased up and down motion of the head, nails dragging more, stopping and laying down ). Know your pet’s limit and make sure get home before it is reached. Your cat's shaky legs while squatting in the litter box, or missing the litter box entirely can be signs of discomfort. Exercise relieves stiffness and increases/maintains mobility but make sure you provide it without causing pain or exhaustion.
Back to Table of Contents
5. Supplements
There are many different types of supplements that have been used to ease inflammation (arthritis defined as inflammation of the joint.) Supplements tend to have less side effects than many pharmaceuticals (drugs) and can also be most helpful in decreasing the dose of medications. That said, most supplements lack good evidence of efficacy and much of their popularity is based on personal experience and reports for peers and clients. Glucosamine, usually combined with chondroitin and avocado/soy unsaponifiables, is a go to supplement for animals. Omega III Fatty Acids ("EPA" and "DHA" found in fish oils as dogs and cats cannot utilize the omega III FAs in flax seed the way humans can), are thought to possibly decrease inflammation at higher doses. Dried milk protein, and curcumin (the ingredient in the spice turmeric) are believed to have anti inflammatory properties as does green lipped mussel extract, whose benefits are probably from its content of omega III FAs. Arnica and so many other supplements are available to minimize inflammation. Ask your vet about what they think of supplements. Often, by the time we see signs of pain, the focus is on more evidence based therapeutics and proper nutrition but certain supplements can play a role in supportive care.
There are many different types of supplements that have been used to ease inflammation (arthritis defined as inflammation of the joint.) Supplements tend to have less side effects than many pharmaceuticals (drugs) and can also be most helpful in decreasing the dose of medications. That said, most supplements lack good evidence of efficacy and much of their popularity is based on personal experience and reports for peers and clients. Glucosamine, usually combined with chondroitin and avocado/soy unsaponifiables, is a go to supplement for animals. Omega III Fatty Acids ("EPA" and "DHA" found in fish oils as dogs and cats cannot utilize the omega III FAs in flax seed the way humans can), are thought to possibly decrease inflammation at higher doses. Dried milk protein, and curcumin (the ingredient in the spice turmeric) are believed to have anti inflammatory properties as does green lipped mussel extract, whose benefits are probably from its content of omega III FAs. Arnica and so many other supplements are available to minimize inflammation. Ask your vet about what they think of supplements. Often, by the time we see signs of pain, the focus is on more evidence based therapeutics and proper nutrition but certain supplements can play a role in supportive care.
6. Heat & Cold Therapy
How relaxing is that lavender filled, microwavable rice pack on your sore neck muscles or the coolness of that bag of frozen peas on a sore knee ? Animals benefit from these simple home therapies as well and often will let you know if cool or warmth feels good (or not). A recommended use for this type of therapy is 15 minutes on, 15 minutes off for about one hour. Be careful with both temperature- you don't want to cause burns or cold damage by placing items directly on bare skin (or over thinning fur.) Elderly pets with thin fur can have compromised capabilities to compensate and their skin can be injured more easily than the skin of youngsters and there are other conditions that can affect your pet's body to tolerate direct temperature therapy. Do not leave a pet unattended with these therapies, especially ones that may have difficulty moving away or communicating discomfort from heat or cold, such as an animals that sleep very soundly, are sedate from side effects of medication, are recovering from surgery and not fully "aware" or have neurological impairment.
Check with your veterinary professional for recommendations of these therapies.
MAKING YOUR OWN:
How relaxing is that lavender filled, microwavable rice pack on your sore neck muscles or the coolness of that bag of frozen peas on a sore knee ? Animals benefit from these simple home therapies as well and often will let you know if cool or warmth feels good (or not). A recommended use for this type of therapy is 15 minutes on, 15 minutes off for about one hour. Be careful with both temperature- you don't want to cause burns or cold damage by placing items directly on bare skin (or over thinning fur.) Elderly pets with thin fur can have compromised capabilities to compensate and their skin can be injured more easily than the skin of youngsters and there are other conditions that can affect your pet's body to tolerate direct temperature therapy. Do not leave a pet unattended with these therapies, especially ones that may have difficulty moving away or communicating discomfort from heat or cold, such as an animals that sleep very soundly, are sedate from side effects of medication, are recovering from surgery and not fully "aware" or have neurological impairment.
Check with your veterinary professional for recommendations of these therapies.
MAKING YOUR OWN:
- Heat pack: fill a sock or cloth sleeve with uncooked rice or flax seed, allowing room for the material to conform to body parts. Sew the sock shut. I would recommend using natural material (cotton) which may be more microwaveable safe and not release weird odors. Always mix after heating and test it on yourself before you place it on your pet.
- Cold pack: In a plastic freezer bag of whichever size you prefer, use a 2:1 water to isopropyl (rubbing) alcohol mixture (purchased at any drug store.) Evacuate as much of the air from the bag before closing it, it makes the liquid better able to conform around body parts. Place it in a second bag to contain any leaks, also evacuating air. Freeze for at least an hour. Be cautious, this gets very, very cold so wrap the bag in a T-shirt and make sure to lift the bag away from bare skin every couple of minutes. This is especially important in sedate or compromised pets such as the elderly or underweight, and especially in small pets that can get hypothermic (cold) quickly.
7. Manual and Complementary Therapies: Acupuncture, Massage, PT and more.
Complementary therapy is used to describe therapies that are outside of the general health care and pharmaceuticals (medication) a pet receives from their primary care vet. Diet, exercise and good nutrition are all complementary and yet very basic and important therapies regular veterinarians often discuss. Other therapies may require additional training or certification by your vet or animal care professional. Manual therapies include all sorts of hands on therapies that help achieve the goal to maximize mobility and function (like PT!)
Acupuncture is a form of therapy where special needles are used on skin to alter nerve signals and on a cellular level, release natural chemicals that call upon the body's own ability for healing. Like any other therapy, some pets respond better than others and there are many factors that can dictate the level of success of acupuncture such as condition, patient temperament, concurrent drug therapies, and individual practitioner technique. One of the benefits of acupuncture is that it doesn't force or bypass the body’s safety mechanisms like drugs can. Acupuncture is one of many alternative therapies available to pets.
Myofascial trigger point therapy uses fingers and/or acupuncture needles to release localized muscle spasm- relieving pain and improving flexibility and range of motion of joints. Many acupuncturist, massage and rehab professionals can address trigger points.
Massage therapy is something you can learn how to do to a certain degree, and there are also animal professionals trained in animal massage therapists. Dogs with hind leg pain are often sore in their shoulders from having to balance weight off their hind ends. Massage, like heat, can improve blood flow and loosen a tight and painful muscle. Be aware that massage done too often, too hard or in the wrong manner can cause injury! Consult a professional and have them teach you the things that are appropriate to do at home.
Cold Laser Therapy is another popular treatment, where light is used to stimulate blood flow and mitochondrial activity, to improve mobility, decrease pain and inflammation at site of both acute (such as a wound or torn ligament) and chronic (such as arthritis.) injury. There are different classes of cold laser with the most effective being a Class IV, especially in larger pets.
Rehabilitation Therapy. Have you ever torn your rotator cuff? Injured an ACL? Did you get PT? Rehab therapy is crucial to maximizing proper healing: minimizing the chances that an acute injury becomes a chronic one or to minimize the pain of a chronic injury. Pets are in luck: physical therapy exists for them too. It is an often overlooked part of pain management. Regaining the ability to use the body can decrease your pet’s dependency for medication. If you cannot afford the time or expense to pursue regular therapy for your pet, consider at least getting a consult with a certified animal rehab therapist, trained specifically for canine and feline musculoskeletal therapy, and be truthful: ask what you could do at home if you can't go into therapy regularly. Controlled water exercise is part of rehab therapy and often a great way to lighten the load on painful joints while giving muscles a way to work out gently- ask for suggestions on the proper way to exercise your pet based on the specific condition. Treadmill therapy can be gentler and less likely to cause injury than uncontrolled swimming. It is important to have a trained therapist determine which type of water exercise is best for your pet's specific issues. Simple range of motion exercises can be of great help to prevent joints and muscles from stiffening up from disuse. Even simple and gentle exercise can be overdone, however, so it is important to have a professional help you determine the level appropriate for your pet.
Chiropractics is another modality for chronic pain. Some techniques used in people can cause trauma to our veterinary patient so make sure you seek the service of practitioners certified in veterinary care or one that works directly with your vet. Laws and regulations vary by state as to who is allowed to work on animals if the practitioner is not a veterinarian.
Naturopathy, homeopathy, herbal medicine and food therapy are available for animals as well. An acupuncturist trained through Traditional Chinese Medicine (TCM) may in some cases also offer TCM herb and nutrition therapy.
Shock Wave therapy, officially extracorporeal shock wave therapy ( ESWT), uses high energy sound waves to heal injuries and/or relieve pain. It is very popular in equine medicine but becoming more popular in small animals. Sedation/anesthesia is necessary for animals to receive this treatment as it is otherwise not tolerated by our animal patients.
There are developing medical therapies such as stem cell injections for injured ligaments, platelet rich plasma for arthritic joints and Nerve Growth Factor antibody therapy (available for cats!!! ).
These are the most popular therapies, and there are more out there!
Back to Table of Contents i
Complementary therapy is used to describe therapies that are outside of the general health care and pharmaceuticals (medication) a pet receives from their primary care vet. Diet, exercise and good nutrition are all complementary and yet very basic and important therapies regular veterinarians often discuss. Other therapies may require additional training or certification by your vet or animal care professional. Manual therapies include all sorts of hands on therapies that help achieve the goal to maximize mobility and function (like PT!)
Acupuncture is a form of therapy where special needles are used on skin to alter nerve signals and on a cellular level, release natural chemicals that call upon the body's own ability for healing. Like any other therapy, some pets respond better than others and there are many factors that can dictate the level of success of acupuncture such as condition, patient temperament, concurrent drug therapies, and individual practitioner technique. One of the benefits of acupuncture is that it doesn't force or bypass the body’s safety mechanisms like drugs can. Acupuncture is one of many alternative therapies available to pets.
Myofascial trigger point therapy uses fingers and/or acupuncture needles to release localized muscle spasm- relieving pain and improving flexibility and range of motion of joints. Many acupuncturist, massage and rehab professionals can address trigger points.
Massage therapy is something you can learn how to do to a certain degree, and there are also animal professionals trained in animal massage therapists. Dogs with hind leg pain are often sore in their shoulders from having to balance weight off their hind ends. Massage, like heat, can improve blood flow and loosen a tight and painful muscle. Be aware that massage done too often, too hard or in the wrong manner can cause injury! Consult a professional and have them teach you the things that are appropriate to do at home.
Cold Laser Therapy is another popular treatment, where light is used to stimulate blood flow and mitochondrial activity, to improve mobility, decrease pain and inflammation at site of both acute (such as a wound or torn ligament) and chronic (such as arthritis.) injury. There are different classes of cold laser with the most effective being a Class IV, especially in larger pets.
Rehabilitation Therapy. Have you ever torn your rotator cuff? Injured an ACL? Did you get PT? Rehab therapy is crucial to maximizing proper healing: minimizing the chances that an acute injury becomes a chronic one or to minimize the pain of a chronic injury. Pets are in luck: physical therapy exists for them too. It is an often overlooked part of pain management. Regaining the ability to use the body can decrease your pet’s dependency for medication. If you cannot afford the time or expense to pursue regular therapy for your pet, consider at least getting a consult with a certified animal rehab therapist, trained specifically for canine and feline musculoskeletal therapy, and be truthful: ask what you could do at home if you can't go into therapy regularly. Controlled water exercise is part of rehab therapy and often a great way to lighten the load on painful joints while giving muscles a way to work out gently- ask for suggestions on the proper way to exercise your pet based on the specific condition. Treadmill therapy can be gentler and less likely to cause injury than uncontrolled swimming. It is important to have a trained therapist determine which type of water exercise is best for your pet's specific issues. Simple range of motion exercises can be of great help to prevent joints and muscles from stiffening up from disuse. Even simple and gentle exercise can be overdone, however, so it is important to have a professional help you determine the level appropriate for your pet.
Chiropractics is another modality for chronic pain. Some techniques used in people can cause trauma to our veterinary patient so make sure you seek the service of practitioners certified in veterinary care or one that works directly with your vet. Laws and regulations vary by state as to who is allowed to work on animals if the practitioner is not a veterinarian.
Naturopathy, homeopathy, herbal medicine and food therapy are available for animals as well. An acupuncturist trained through Traditional Chinese Medicine (TCM) may in some cases also offer TCM herb and nutrition therapy.
Shock Wave therapy, officially extracorporeal shock wave therapy ( ESWT), uses high energy sound waves to heal injuries and/or relieve pain. It is very popular in equine medicine but becoming more popular in small animals. Sedation/anesthesia is necessary for animals to receive this treatment as it is otherwise not tolerated by our animal patients.
There are developing medical therapies such as stem cell injections for injured ligaments, platelet rich plasma for arthritic joints and Nerve Growth Factor antibody therapy (available for cats!!! ).
These are the most popular therapies, and there are more out there!
Back to Table of Contents i
8. Medication
Pain is a complex process involving the site of injury (affected tissue) and signals to and from the nerves through the spinal cord to the brain. Different drugs target different sources and different types of pain. There isn't one magic pill. Medical management of chronic pain involves a "multi-modal" approach for many factors, including how the brain perceives chronic pain and how the pain signal is transmitted through the spinal cord. Often it is finding the combination of therapies that works best for YOUR pet. Vets may use a combination of non-steroidal anti-inflammatory analgesics/drugs (NSAIDs), "pain killers"-analgesics that don't have anti-inflammatory properties, such as opioids, medications that affect the way the nerves signal, like gabapentin, and/or drugs that provide the body with building blocks for healthy joints like Adequan. There are even certain antidepressants that can aid to relieve pain. Some of the drug choices your vet makes will depend on what your pet's body can handle. There are side effects to all drugs and your vet has to figure out the best combination while balancing the safety of those drugs. Your vet will make an informed decision with the aid of regular exams, blood work and your feedback. We are really excited that Solensia has finally been approved in the US for pain caused by osteoarthritis in cats. This injectable drug administered at the vet clinic uses monoclonal antibody (mAb) technology to prevent communication by pain receptors, resulting in decreased pain sensation. The recommendations is for once a month injections and we often will start with two treatments to evaluate how effective that modality is for an individual patient. We are eagerly waiting the release of Librela for dogs, which has just been approved in the US.
Remember: Always " Check with your vet" before you administer new supplements, add or switch medications.
Back to Table of Contents
Pain is a complex process involving the site of injury (affected tissue) and signals to and from the nerves through the spinal cord to the brain. Different drugs target different sources and different types of pain. There isn't one magic pill. Medical management of chronic pain involves a "multi-modal" approach for many factors, including how the brain perceives chronic pain and how the pain signal is transmitted through the spinal cord. Often it is finding the combination of therapies that works best for YOUR pet. Vets may use a combination of non-steroidal anti-inflammatory analgesics/drugs (NSAIDs), "pain killers"-analgesics that don't have anti-inflammatory properties, such as opioids, medications that affect the way the nerves signal, like gabapentin, and/or drugs that provide the body with building blocks for healthy joints like Adequan. There are even certain antidepressants that can aid to relieve pain. Some of the drug choices your vet makes will depend on what your pet's body can handle. There are side effects to all drugs and your vet has to figure out the best combination while balancing the safety of those drugs. Your vet will make an informed decision with the aid of regular exams, blood work and your feedback. We are really excited that Solensia has finally been approved in the US for pain caused by osteoarthritis in cats. This injectable drug administered at the vet clinic uses monoclonal antibody (mAb) technology to prevent communication by pain receptors, resulting in decreased pain sensation. The recommendations is for once a month injections and we often will start with two treatments to evaluate how effective that modality is for an individual patient. We are eagerly waiting the release of Librela for dogs, which has just been approved in the US.
Remember: Always " Check with your vet" before you administer new supplements, add or switch medications.
Back to Table of Contents